Comprehensive Insights into Blood Test Markers Essential for Accurate Arthritis Diagnosis
Gaining a thorough understanding of Arthritis blood test markers is crucial for achieving precise diagnoses and effective management of arthritis, a widespread condition impacting millions across the United Kingdom. These markers act as specific biological indicators that provide information about the presence of inflammation and autoimmune responses within the body. They play a significant role in offering insights into the type and severity of arthritis a patient may be experiencing. By enhancing our grasp of these markers, both patients and healthcare professionals can navigate the complexities associated with arthritis management more effectively, ultimately leading to improved health outcomes and a significantly enhanced quality of life for those affected by this debilitating condition.
Why Understanding Arthritis Blood Test Markers is Vital for Accurate Diagnosis
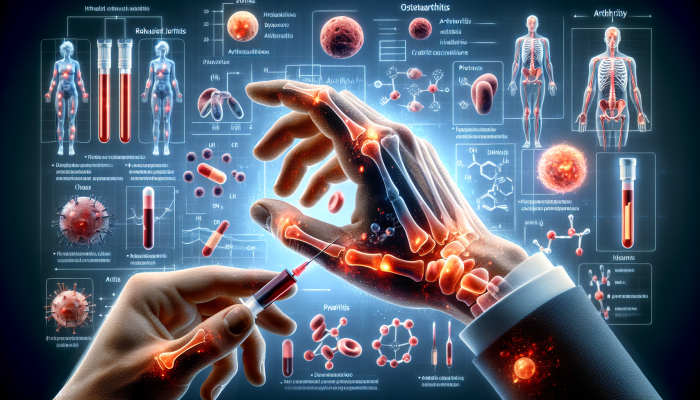
Arthritis blood test markers are biochemical substances found in the bloodstream that provide vital information concerning the presence and effects of arthritis on the body. This extensive range of markers includes various proteins, antibodies, and molecules that demonstrate changes in concentration when the body experiences inflammation or joint damage. Their primary function is to assist in diagnosing multiple forms of arthritis, including rheumatoid arthritis, osteoarthritis, and psoriatic arthritis. Each specific type of arthritis typically presents with a unique set of markers, which healthcare professionals evaluate during blood tests, making the understanding of these markers essential for timely and accurate diagnosis.
When patients exhibit symptoms commonly associated with arthritis, such as joint pain, swelling, and stiffness, medical practitioners frequently recommend blood tests to evaluate these markers. The insights gained from these tests are critical in guiding clinicians to formulate the most effective treatment plans and to monitor their efficacy throughout the treatment process. It is essential to recognize that while these markers provide valuable diagnostic information, they should not be viewed in isolation. Healthcare providers must take into account the patient’s complete clinical picture, which includes symptoms, medical history, and results from other diagnostic tests, to make well-informed and accurate treatment decisions.
Detailed Examination of Various Arthritis Blood Test Markers
The spectrum of arthritis blood test markers is vast, comprising numerous indicators specifically designed for different forms of arthritis. For instance, rheumatoid factor (RF) is routinely measured in patients suspected of having rheumatoid arthritis. Elevated RF levels typically suggest an autoimmune response, indicating that the body is mistakenly attacking its own tissues. Another essential marker is the anti-cyclic citrullinated peptide (anti-CCP) antibody, which is highly specific to rheumatoid arthritis and can sometimes be detected even before clinical symptoms manifest.
In addition to these specific markers, the erythrocyte sedimentation rate (ESR) is a well-established test conducted in the UK to assess general inflammation levels within the body. While this test is not exclusive to arthritis, an elevated ESR can signal the existence of inflammatory processes associated with various forms of arthritis. A comprehensive understanding of the significance of these markers fosters a more nuanced diagnostic approach, enabling healthcare professionals to create treatment strategies that specifically target the type of arthritis affecting the patient.
The Essential Role of Regular Testing in Effective Arthritis Management
Regular testing for arthritis blood test markers is vital for both initial diagnosis and ongoing management of the condition. Given that arthritis can be progressive, monitoring these markers allows healthcare providers to track changes in a patient’s condition over time. Routine blood tests enable clinicians to evaluate the effectiveness of treatments, make necessary adjustments, and identify potential complications early, which is crucial for preserving joint health and enhancing overall wellbeing.
Patients in the UK are strongly encouraged to maintain clear communication with their healthcare providers regarding the frequency of testing needed. For some individuals, it may be advisable to undergo testing every few months, particularly during the initial treatment phase or when symptoms fluctuate. Regular monitoring ensures that any increases in inflammatory markers are promptly addressed, which can help prevent further joint damage and significantly improve the quality of life for individuals living with arthritis.
Interpreting and Understanding Results from Arthritis Blood Tests

Deciphering the results of arthritis blood tests requires a nuanced understanding of the levels and patterns of various markers. Normal levels can fluctuate significantly among individuals, meaning that what may be elevated for one person may not be for another. Therefore, it is crucial to consult with a knowledgeable healthcare professional who can contextualize these results within the broader framework of the patient’s overall health, factoring in lifestyle choices and medical history.
For instance, if a patient’s rheumatoid factor levels are elevated but they do not show symptoms typically associated with rheumatoid arthritis, further investigation may be necessary to rule out false positives or other underlying conditions. Similarly, correlating blood test results with clinical symptoms is vital for achieving an accurate diagnosis. A thorough assessment by a rheumatologist can lead to a clearer understanding of what the test results indicate for the patient’s treatment plan and overall health strategy.
Recognising the Limitations of Arthritis Blood Test Markers
While arthritis blood test markers provide valuable insights, they are not without limitations. A significant drawback is that some markers may occur in individuals without arthritis or may not be elevated in every case of the disease. This variability underscores the necessity of utilizing these tests alongside other diagnostic methods, such as imaging studies and physical examinations, to create a comprehensive view of the patient’s condition and specific needs.
Additionally, some patients may exhibit symptoms of arthritis without corresponding changes in blood test markers, posing challenges for healthcare professionals. In such instances, clinicians may need to rely on clinical judgment and patient history to arrive at a diagnosis. Therefore, while arthritis blood test markers are essential tools in the diagnostic arsenal, they should be integrated into a broader diagnostic strategy rather than solely relied upon for clinical decisions.
Key Blood Test Markers Frequently Used for Arthritis Diagnosis in the UK
In the UK, a variety of blood test markers are routinely employed to diagnose and monitor arthritis. Cultivating a comprehensive understanding of these markers empowers patients, enabling them to engage more effectively in their healthcare journey and ensuring they are well-informed about the tests relevant to their condition.
Rheumatoid Factor (RF): A Critical Marker for Arthritis Diagnosis
Rheumatoid factor (RF) is one of the most frequently tested markers in the UK for diagnosing rheumatoid arthritis. This autoantibody can be detected in the bloodstream and is often linked with the presence of inflammation and joint damage. Elevated RF levels can indicate an ongoing autoimmune process leading to the destruction of joint tissues.
However, it is essential to understand that while RF is a significant marker, it is not exclusively indicative of rheumatoid arthritis. Increased RF levels can also manifest in other conditions such as Sjögren’s syndrome, and even in some healthy individuals. Therefore, a positive RF test should be interpreted with caution and always in conjunction with clinical symptoms and other diagnostic assessments. In the context of ongoing monitoring, any fluctuations in RF levels can provide valuable insights into treatment effectiveness and disease progression, assisting healthcare providers in adapting their treatment strategies as necessary.
Anti-Cyclic Citrullinated Peptide (Anti-CCP): A Key Indicator for Early Detection
The anti-cyclic citrullinated peptide (anti-CCP) antibody serves as another crucial marker for diagnosing rheumatoid arthritis. This antibody is highly specific to the condition, making it a more definitive indicator than RF. The presence of anti-CCP antibodies can sometimes be detected years before the clinical onset of rheumatoid arthritis, presenting a vital opportunity for early intervention that can significantly influence long-term outcomes.
In practical terms, testing for anti-CCP antibodies can lead to more accurate diagnoses, enabling healthcare providers to implement treatment strategies sooner in the disease process. This proactive approach is critical for effectively managing rheumatoid arthritis, as early treatment can greatly enhance long-term outcomes and improve the quality of life for patients. Understanding the implications of a positive anti-CCP test empowers patients to take an active role in managing their health and making informed decisions regarding their treatment options.
Erythrocyte Sedimentation Rate (ESR): A General Indicator of Inflammation
The erythrocyte sedimentation rate (ESR) is a non-specific marker commonly utilized in the UK to assess inflammation levels within the body. While it does not differentiate between types of arthritis, a high ESR can indicate the presence of inflammatory processes, making it a valuable tool when interpreted alongside other specific markers.
In practice, monitoring ESR is often employed to gauge disease activity in patients with arthritis. A declining ESR may signal that inflammation is subsiding and that treatment is effective, while an increasing ESR could indicate a flare-up or worsening condition. Although this marker is not definitive on its own, it provides essential context when assessed alongside clinical symptoms and other test results. The ability to track ESR over time can assist patients and healthcare providers in understanding treatment efficacy and adapting management plans accordingly, ensuring optimal health outcomes.
Expertly Navigating the Interpretation of Arthritis Blood Test Results
Interpreting arthritis blood test results is a complex process that necessitates careful consideration of various factors, including the specific markers tested and the patient’s overall condition. An informed approach to interpreting these results can significantly influence treatment decisions and patient outcomes, ultimately shaping the trajectory of arthritis management.
Establishing Normal Versus Abnormal Levels in Blood Tests
Determining what constitutes normal and abnormal levels of arthritis blood test markers is not always straightforward. Each marker possesses its own reference range, which can vary based on factors such as age, sex, and laboratory standards. Understanding what constitutes normal can assist both patients and healthcare professionals in making informed decisions regarding diagnosis and treatment.
For example, rheumatoid factor levels that fall within the normal range suggest that the autoimmune component of rheumatoid arthritis may not be present. Conversely, elevated levels may prompt further investigation. However, it is crucial to recognize that a single test result should not dictate a diagnosis. Instead, healthcare providers must consider the entirety of a patient’s clinical presentation, including symptoms, medical history, and results from other diagnostic tests to achieve a well-rounded understanding of the patient’s health status.
Correlating Blood Test Results with Symptoms for Accurate Diagnosis
Interpreting blood test results in the context of clinical symptoms is essential for achieving an accurate diagnosis and treatment plan. For instance, a patient may exhibit elevated levels of certain markers but may not display any noticeable symptoms. In such cases, healthcare professionals might need to conduct further assessments to determine the relevance of the test results.
A comprehensive evaluation involves examining how blood test results correlate with pain levels, joint mobility, and other symptomatic indicators. For example, if a patient shows high levels of anti-CCP antibodies but reports minimal symptoms, the healthcare provider may recommend a watchful waiting approach rather than immediate treatment. This correlation between laboratory results and clinical symptoms allows for a more tailored and effective management strategy, enhancing the patient’s overall care and experience.
The Importance of Consulting Healthcare Professionals for Interpreting Results
In the UK, consulting healthcare professionals such as rheumatologists or general practitioners is vital for interpreting and acting on arthritis blood test results. These specialists possess the expertise to contextualize test findings and recommend appropriate next steps. Patients are encouraged to engage in open discussions with their healthcare providers regarding their test results, as a collaborative approach can lead to a more thorough understanding of their condition.
Rheumatologists, in particular, can provide insights into the implications of specific markers and guide patients through the complexities of arthritis management. They may suggest additional tests or imaging studies to confirm a diagnosis or evaluate the extent of joint damage. Furthermore, having a clear understanding of the results can empower patients to make informed decisions about their treatment options and actively participate in their healthcare journey, fostering a sense of ownership over their health outcomes.
NHS Guidelines for Arthritis Blood Testing Protocols
The NHS plays a crucial role in guiding patients through the process of arthritis blood testing. Familiarity with these guidelines can help individuals understand when to seek testing and what to expect during the diagnostic journey, ensuring a smoother experience overall.
Recognizing the Right Timing for Arthritis Testing
NHS guidelines recommend conducting blood tests when patients exhibit symptoms indicative of arthritis, such as persistent joint pain, swelling, or stiffness. Early testing can facilitate timely diagnosis and intervention, ultimately improving long-term outcomes for individuals suffering from arthritis and enhancing their quality of life.
In specific scenarios, patients may be referred for testing by their GP when there is a suspicion of arthritis or if they are experiencing significant joint-related symptoms. Awareness of these guidelines empowers patients to advocate for themselves and seek the necessary testing to ensure they receive prompt and effective care, allowing for better management of their condition.
Determining Optimal Testing Frequency for Effective Management
The frequency of arthritis blood testing in the UK is typically determined by the type of arthritis, the patient’s condition, and the treatment plan. NHS guidelines suggest that regular testing may be necessary for patients with active inflammatory arthritis to continuously monitor disease progression and treatment efficacy.
For instance, patients newly diagnosed with rheumatoid arthritis might undergo testing every few months during the initial treatment phase. Once the condition stabilizes, the frequency of testing may be adjusted accordingly. Regular follow-ups with healthcare professionals ensure that testing schedules align with the patient’s health status and treatment goals, facilitating optimal management and improved health outcomes.
Accessing NHS Testing Services for Comprehensive Arthritis Evaluation
Patients in the UK can access arthritis blood testing services through the NHS, usually requiring a referral from their GP. The process typically involves an initial consultation, where the healthcare provider will assess symptoms and determine the necessity for testing. This systematic approach ensures that patients receive appropriate evaluations tailored to their specific needs.
Once referred, patients can expect to visit a local laboratory for blood collection. The results are generally processed and made available within a few days, allowing for timely decision-making regarding treatment options. Understanding how to access these services enables patients to navigate the healthcare system effectively, ensuring they receive the necessary evaluations promptly and efficiently.
Guidance on Interpreting Test Results within the NHS Framework
The NHS provides guidance on interpreting arthritis blood test results, which is essential for both patients and healthcare providers alike. Clear communication regarding test outcomes can significantly influence treatment decisions and enhance patient engagement in their care, ensuring that individuals comprehend their health status.
Healthcare professionals are trained to explain the significance of various markers and their implications for arthritis management. Patients are encouraged to ask questions and seek clarification to ensure they fully understand their results. This collaborative approach fosters a supportive environment for patients, enabling them to make informed choices about their health and treatment options, ultimately leading to enhanced patient satisfaction and improved outcomes.
Exploring Private Arthritis Blood Testing Options in the UK
In addition to NHS services, private arthritis blood testing alternatives are available in the UK, offering patients an alternative route to accessing diagnostic evaluations. Understanding the benefits and considerations associated with private testing can empower individuals to make informed health decisions regarding their care and management strategies.
The Advantages of Opting for Private Testing Services
Private testing for arthritis blood markers can provide numerous benefits, including expedited results and a more comprehensive range of tests. Patients choosing private testing often appreciate the reduced waiting times associated with private healthcare, enabling quicker diagnoses and allowing for timely adjustments to treatment plans.
Moreover, private clinics may offer access to a wider variety of tests, including specialized markers that are not typically included in standard NHS panels. This can be particularly advantageous for individuals seeking a more detailed assessment of their condition. The ability to receive prompt results and more in-depth testing can significantly enhance the overall patient experience and contribute to better management of arthritis, fostering a sense of control over one’s health.
Financial Considerations for Private Testing Services
While private arthritis blood testing presents distinct advantages, patients should be aware of the associated costs. Private testing can often be more expensive than NHS services, and prices may vary considerably depending on the clinic and the specific tests required.
Patients contemplating private testing are advised to conduct thorough research into their options and inquire about pricing before making a decision. Understanding the costs related to private testing can help individuals weigh the benefits against their budget, ensuring they make an informed choice that aligns with their healthcare needs and financial situation, ultimately enhancing their overall satisfaction with their care.
Selecting a Reliable Private Clinic for Accurate Blood Testing
Choosing a reputable private clinic for arthritis blood testing is essential for ensuring accurate and reliable results. Patients are encouraged to seek clinics that are accredited and have a proven track record in conducting arthritis-related tests, ensuring they receive high-quality care.
Reviews and recommendations from other patients can provide valuable insights into the quality of care offered by a private clinic. Additionally, healthcare professionals can assist patients in identifying reputable facilities that specialize in arthritis testing. Making an informed choice about where to undergo testing can significantly influence the quality of the patient experience and the reliability of the results obtained, ultimately contributing to better health outcomes.
Interpreting Results from Private Blood Tests for Informed Decision-Making
Interpreting results from private arthritis blood tests can be complex, necessitating discussions with a healthcare professional for clarity and context. Private clinics often provide detailed reports, encompassing a multitude of markers and their corresponding levels, but without appropriate context, these results can be challenging to interpret accurately.
Patients are encouraged to consult with their healthcare providers to fully grasp the significance of their test results and the implications for their treatment plans. This collaborative approach ensures that patients are well-informed and empowered to make educated decisions regarding their health, ultimately leading to improved management of their arthritis.
Technological Advancements in Arthritis Blood Testing: A Future-Focused Perspective
The field of arthritis blood testing is continually evolving, with significant innovations in technology and testing methods emerging in the UK. These breakthroughs are transforming the way arthritis is diagnosed and managed, providing hope for more effective treatments and improved patient outcomes as research progresses.
Innovative Markers and Advanced Testing Techniques
Recent advancements in arthritis blood testing technology include the development of new markers with enhanced specificity and sensitivity. Researchers are actively investigating novel biomarkers that could provide insights into the underlying mechanisms of arthritis, potentially leading to earlier diagnosis and more targeted therapies tailored to individual patient needs.
Furthermore, improved testing techniques, such as high-throughput assays and more sophisticated imaging technologies, are enhancing the accuracy of results and the ability to diagnose arthritis at earlier stages. These innovations empower healthcare providers to obtain more detailed information regarding a patient’s condition, thereby informing better treatment decisions and strategies tailored to individual needs and circumstances.
The Impact of Technological Innovations on Diagnosis and Treatment Strategies
The influence of advancements in blood testing technology on diagnosis and treatment is profound and far-reaching. With the capability to identify specific markers associated with different types of arthritis, healthcare providers can personalize treatment plans to meet the unique needs of patients, leading to more effective management.
For instance, patients with early-stage rheumatoid arthritis may benefit from targeted therapies that focus on their specific biomarkers, thereby reducing the risk of joint damage and significantly improving long-term outcomes. The integration of new technologies into clinical practice promises to enhance the overall quality of care for patients, paving the way for more effective management of their conditions and improving their overall wellbeing.
Future Prospects for Advancements in Arthritis Blood Testing
The future of arthritis blood testing in the UK appears promising, with ongoing research and development aimed at further enhancing diagnostic capabilities and treatment options. As new markers and testing techniques continue to emerge, the potential for improved patient outcomes grows exponentially.
Continued investment in research is crucial for uncovering the complexities of arthritis and developing innovative solutions for diagnosis and treatment. By harnessing the power of advancing technologies, healthcare providers can better serve patients, ensuring they receive timely, accurate diagnoses and optimized treatment plans tailored to their unique needs, ultimately enhancing their quality of life.
The Interplay Between Lifestyle Choices and Arthritis Blood Testing
While medical interventions are critical for managing arthritis, lifestyle factors also play a substantial role in overall health and wellbeing. Recognizing how lifestyle choices can affect arthritis and understanding the importance of regular blood tests can empower patients to take control of their health journey, leading to improved management and outcomes.
The Impact of Diet and Nutrition on Effective Arthritis Management
Dietary choices can significantly influence inflammation levels within the body, which is particularly vital for individuals living with arthritis. Research indicates that certain foods, especially those high in omega-3 fatty acids, can help reduce inflammation and promote joint health. Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall wellbeing and potentially alleviate some arthritis symptoms, leading to an enhanced quality of life.
Moreover, patients should collaborate with healthcare professionals, including dietitians, to create personalized nutrition plans tailored to their specific needs and health goals. Regular blood testing can also assist in monitoring nutrient levels and identifying any deficiencies that may impact overall health, ensuring that dietary choices positively contribute to arthritis management and overall wellbeing.
Exercise and Physical Activity: Crucial for Joint Health
Engaging in regular physical activity is essential for managing arthritis and maintaining joint functionality. Participating in low-impact exercises, such as swimming or walking, can help strengthen the muscles surrounding the joints, enhance flexibility, and reduce stiffness. Furthermore, exercise offers additional benefits by improving overall physical and mental health, which is vital for individuals coping with chronic conditions.
Patients should consult with healthcare providers or physiotherapists to develop safe and effective exercise regimens suited to their individual capabilities and needs. By incorporating consistent activity into their lifestyles, patients can positively influence their arthritis management and enhance their overall quality of life, supporting their physical and emotional wellbeing.
Managing Stress for Optimal Health Outcomes
Stress can exacerbate symptoms of arthritis, making effective stress management techniques essential for patients. Approaches such as meditation, yoga, and deep-breathing exercises can help alleviate stress and improve overall emotional wellbeing. By effectively managing stress levels, individuals may experience improved symptoms and enhanced quality of life, positively influencing their arthritis management.
Regular blood testing can also help identify any potential stress-related physiological changes within the body. By understanding how stress impacts their health, patients can implement effective stress management techniques into their daily routines, ultimately benefiting their arthritis management and overall health.
The Vital Importance of Open Communication with Healthcare Providers
Maintaining clear communication with healthcare providers is fundamental for effectively managing arthritis. Patients should feel empowered to discuss their symptoms, concerns, and lifestyle choices openly, as this collaborative approach can lead to more tailored and effective care that meets their individual needs.
Regular blood testing provides an opportunity for patients to engage in discussions about their health progress and treatment outcomes. By fostering a supportive relationship with healthcare professionals, patients can navigate the complexities of arthritis management with greater confidence, ensuring they receive the best possible care and support for their condition.
Adapting Lifestyle Choices for Enhanced Health Outcomes
Ultimately, taking a proactive approach towards lifestyle changes can significantly improve the management of arthritis. By focusing on diet, exercise, stress management, and maintaining open communication with healthcare providers, patients can greatly influence their health outcomes. Regular monitoring through blood tests can provide valuable insights into how lifestyle choices impact arthritis, empowering individuals to make informed decisions for their wellbeing and enhancing their overall health and quality of life.
Answers to Common Questions About Arthritis Blood Testing
What are the primary markers associated with arthritis blood tests?
Arthritis blood test markers are biological indicators present in the blood that assist in diagnosing and monitoring various types of arthritis by revealing signs of inflammation or autoimmune activity, which helps tailor treatment strategies effectively.
How are these markers utilized in the diagnostic process?
These markers are tested to assess the presence of arthritis and determine its type, aiding healthcare professionals in customizing treatment plans based on specific findings and individual patient needs.
Why is regular testing crucial for arthritis patients?
Regular testing allows for ongoing monitoring of disease progression and treatment effectiveness, enabling timely adjustments to management strategies as required, which significantly enhances patient outcomes and quality of life.
What should I do if my blood test results are abnormal?
Consult your healthcare provider to discuss the implications of abnormal results and explore potential next steps in your arthritis management, ensuring a comprehensive approach to your care.
How often should I undergo blood testing for arthritis?
The frequency of testing varies depending on the type of arthritis and individual health status; your healthcare provider can recommend an appropriate schedule tailored to your specific needs and treatment goals.
What is the significance of rheumatoid factor in diagnosis?
Rheumatoid factor (RF) is an autoantibody indicating an autoimmune response, commonly used to diagnose rheumatoid arthritis and assess disease activity, helping to inform treatment decisions.
Are there limitations to relying on blood testing for arthritis?
Yes, arthritis blood test markers can yield false positives or negatives and should be interpreted alongside clinical symptoms and other diagnostic tools for accuracy, ensuring a well-rounded understanding of the patient’s condition.
Can lifestyle changes affect my arthritis blood test results?
Yes, lifestyle factors such as diet, exercise, and stress management can influence inflammation levels and overall health, ultimately impacting blood test results and informing treatment strategies.
What role does private testing play in arthritis management?
Private testing offers quicker results and potentially more comprehensive panels of tests, allowing for more tailored healthcare approaches to effectively managing arthritis and improving patient satisfaction.
How can I access NHS arthritis testing services?
NHS testing services can be accessed through GP referrals, where patients can undergo blood tests at local laboratories specifically for arthritis assessment, ensuring timely and effective care.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article: Arthritis Blood Test Markers Explained: Your Essential Guide appeared first on: https://ezbloodtest.com
The Article Arthritis Blood Test Markers: Essential Guide Explained Was Found On https://limitsofstrategy.com
The Article Arthritis Blood Test Markers: A Comprehensive Overview First Appeared ON
: https://ad4sc.com
Comments are closed